Cost minimization analysis of neoadjuvant treatment of luminal B HER2/neu-negative breast cancer: chemotherapy versus hormone therapy
Artemenko M.V., Bondarenko I.M., Zavizion V.F., Avierin D.I.
Summary. In 2022, there were 2,296,840 registered cases of breast cancer (BC) worldwide and 12,335 in Ukraine. A significant number of patients with early and locally advanced BC require neoadjuvant treatment. In the treatment of luminal B HER2/neu-negative BC, chemotherapy is more commonly used. However, data from recent randomized clinical trials indicate identical efficacy for such cases with neoadjuvant endocrine therapy. Moreover, endocrine therapy has a more favorable toxicity profile, is better tolerated by patients, does not require hospitalization, and is significantly cheaper than chemotherapy. This fact is significant in Ukraine in recent years, where, under wartime conditions, the country and its population have limited financial resources for treatment. The aim of the study was a pharmacoeconomic comparison of the cost of neoadjuvant chemotherapy and neoadjuvant endocrine therapy. Object and Methods. The «cost-minimization» method was applied to conduct the study. In calculating the difference in costs between the two treatment methods, both direct costs (the cost of providing medical care to one person, the cost of therapeutic agents, including agents used for premedication and prevention of the most common manifestations of treatment toxicity, costs of laboratory tests) and indirect costs, primarily the costs of laboratory tests and loss of working capacity and associated losses, were taken into account. Results of the Study. The cost of treatment with standard dose-intensive adjuvant regimens was considered: 4 courses of doxorubicin with cyclophosphamide every 2 weeks followed by 4 courses of paclitaxel every 2 weeks or followed by 12 weekly infusions of paclitaxel, and 6 courses of the combination of docetaxel with cyclophosphamide. These were compared with the cost of treatment with aromatase inhibitors both in monotherapy in menopausal patients and combination with synthetic analogs of luteinizing hormone-releasing hormone in premenopausal women. Depending on the choice of drugs, endocrine therapy is cheaper compared to the recommended international guidelines for neoadjuvant chemotherapy regimens by about 30,000 UAH to approximately 70,000 UAH. Conclusions. With practically identical immediate results of neoadjuvant chemo- and endocrine therapy for early luminal B HER2/neu-negative BC, and taking into account the pharmacoeconomic analysis by the «cost-minimization» method, endocrine therapy is the treatment of choice. It allows significant savings in treatment costs, which is extremely important in financial and economic hardship. However, one cannot rely solely on the results of pharmacoeconomic calculations, as long-term treatment outcomes have yet to be thoroughly studied. Therefore, when choosing the tactics of neoadjuvant treatment, a multidisciplinary team should consider a multifactorial analysis of each patient.
Received 19.11.2024
Accepted for publication 3.12.2024
DOI: 10.32471/clinicaloncology.2663-466X.56-4.33629
In 2022, approximately 2,296,840 cases of BC in women were registered worldwide. The countries leading in the number of cases were China (357,161), the USA (274,375), and India (192,020). The age-standardized incidence rate was highest in France (105.4 per 100,000 women), followed by the USA (95.9 per 100,000) in second place, and the United Kingdom (94.0 per 100,000) in third place [1]. In the same year, Ukraine registered 12,335 cases of BC, with the highest numbers reported in the Dnipro (1,339), Lviv (906), Odesa (846), Kyiv (701) regions, and the city of Kyiv (1,260) [2]. Possibly due to the war in Ukraine, the standardized incidence rate (world standard) for BC in 2022 is currently unknown or unpublished, but in 2021, it was 43.2 per 100,000 female population of the country [3].
Among molecular subtypes, the so-called luminal A (50–60% of all BC cases) and luminal B, which is further divided into HER2/neu-negative (15–20% of all BC cases) and HER2/neu-enriched (10–15%), predominate [4].
Today, for a significant cohort of both locally advanced and localized BC, the standard method of treatment is the so-called neoadjuvant therapy. In most cases, this approach primarily allows for downstaging, significantly increasing the possibility of using organ-preserving surgical technologies. Simultaneously, it demonstrates the tumor’s sensitivity to the applied treatment and influences the choice of adjuvant therapy. While endocrine therapy is preferred for luminal A, chemotherapy is often used for luminal B. Data from many clinical studies demonstrate that chemo- and hormone therapy have almost identical clinical efficacy and provide equal opportunities for performing organ-preserving surgeries [5].
The National Comprehensive Cancer Network (NCCN) recommendations regarding adjuvant or neoadjuvant use of chemotherapy for HER2/neu-negative cancer do not differentiate the choice of regimens based on triple-negative, luminal A, or luminal B HER2/neu-negative subtypes. The proposed regimens include dose-dense administration of 4 courses of doxorubicin with cyclophosphamide (AC), followed by 4 courses of paclitaxel (T) every 2 weeks or 12 weekly infusions at the appropriate dosage. Another preferred regimen is 4–6 courses of a combination of docetaxel with cyclophosphamide. In some instances, the use of pembrolizumab with paclitaxel and carboplatin for 4 courses, followed by 4 courses of pembrolizumab, doxorubicin, and cyclophosphamide every 3 weeks, maybe recommended [6]. European Society for Medical Oncology (ESMO) also recommends the use of chemotherapy for neoadjuvant purposes [7].
American Society of Clinical Oncology (ASCO) allows hormone therapy for postmenopausal patients with hormone-sensitive, HER2/neu-negative BC to downstage the disease [8]. However, while multigene tests such as Oncotype DX, MammaPrint, Breast Cancer Index, and EndoPredict [9] exist for selecting methods of adjuvant systemic therapy, such tests are not used for choosing neoadjuvant treatment. Nonetheless, invaluable experience gained from clinical trials like ACOSOG-Z1031, IMPACT, and POETIC has indicated the possibility of using a cheap yet sufficiently effective laboratory method to monitor the effectiveness of neoadjuvant hormone therapy by studying the proliferation marker Ki-67. If the treatment is effective, Ki-67 decreases after just 2 weeks of hormone therapy, whereas clinical and radiological signs of positive dynamics may only become noticeable after several courses [10–12].
A feature of chemotherapy is that it generally has a significant number of adverse effects that complicate its use and require appropriate management. The development of toxic complications, in turn, may prompt dose reductions or even discontinuation of treatment [13]. In contrast, endocrine therapy has a more favorable toxicity profile, is better tolerated than chemotherapy, and has less impact on patients’ quality of life, at least during neoadjuvant treatment [14].
Since 2014, a bloody war has been ongoing in Ukraine, which, on February 24, 2022, escalated into a full-scale invasion. This has led not only to catastrophic losses of human resources but also to an extraordinary decline in economic indicators and, accordingly, the country’s financial capabilities, which worsen each day the war continues. At the same time, the cost of even standard medical procedures, medications, salaries for medical personnel, and other treatment-related expenses is constantly increasing. The capabilities of the National Health Service of Ukraine to finance expensive treatment regimens are limited. The population’s ability to independently fund their treatment is also catastrophically decreasing. Therefore, the search for cheaper technologies that can deliver the same results as generally accepted but more expensive ones is highly relevant. Considering that neoadjuvant endocrine therapy for luminal B BC, with proper monitoring of tumor response, provides the same opportunities for performing organ-preserving surgeries as chemotherapy, according to clinical studies, the implementation of this technology can be considered a justified option to reduce treatment costs, which, it seems, does not harm long-term outcomes. This «seems» still requires additional research by tracking relapse-free and overall survival results, necessitating extra time.
The study aims to compare the cost of neoadjuvant chemotherapy and neoadjuvant endocrine therapy using the «cost-minimization» method.
For the calculations, the following formula was applied:
CMA = (DC1 + IC1) − (DC2 + IC2),
where CMA is the indicator of the cost difference between the two treatment methods; DC1 is the direct costs when using the first treatment method; IC1 is the indirect costs when using the first treatment method; DC2 and IC2 are the direct and indirect costs, respectively, when using the second treatment method [15].
Direct treatment costs can be considered the cost of providing medical care to one person, as their calculation includes fixed, variable, average, and marginal costs [16], which include personnel costs, utility expenses, etc. Medications are financed separately; the cost of drugs for treating a specific nosological unit is not included in the base rate.
The base rate for the readiness to provide medical care to one person over a year is 36,807 UAH annually. Considering the adjustment coefficient of 0.97 for patients over 18 years old, giving care to one person in a hospital is estimated at 35,702.8 UAH per year, and outpatient care at 25,764.9 UAH per year [17].
Due to the lack of reliable information in the public domain, it was impossible to calculate the cost of drugs obtained by hospitals through state procurements, sponsorship supplies, etc. Therefore, the calculation was performed considering the minimum prices based on data from the websites tabletki.ua [18], medbrowse.com.ua [19], and apteka911.ua [20]. The drug information was verified on the website likicontrol.com.ua [21].
We’ll adopt the standard approach of calculating doses in mg/m² for calculating the cost of chemotherapy drugs. We’ll consider an average body surface area of 1.9 m². So, when using the dose-dense AC regimen, the patient will receive every 2 weeks 114 mg of doxorubicin (60 mg per 1 m²) and 1,140 mg of cyclophosphamide (600 mg per 1 m²). A total of 4 such infusions will be administered. According to medbrowse.com.ua [19], the average price of doxorubicin 100 mg is 1,115 UAH, 50 mg is 627 UAH, 25 mg is 576 UAH, and 10 mg is 140 UAH.
It should be noted that the cost of drugs from well-known brands may significantly exceed the amounts indicated. If these packaging options are available, the optimal is to use 1 vial of 100 mg and 2 of 10 mg. Thus, the total cost of doxorubicin for 1 course of treatment is at least 1,395 UAH. If the 100 mg packaging is unavailable, 2 vials of 50 mg are used, which increases the drug cost to 1,530 UAH.
According to apteka911.ua [20], the approximate prices for cyclophosphamide 1,000 mg are 1,650 UAH, 500 mg is 925 UAH, 200 mg is 330 UAH, and 100 mg is 165 UAH. So, when using 1 vial of 1,000 mg and 1 vial of 200 mg, the cost of the drug for 1 course will be about 1,980 UAH, and when using 2 vials of 500 mg instead of 1 of 1,000 mg, the cost of the drug increases to 2,180 UAH.
Thus, the minimum cost of chemotherapy drugs alone for 1 course of treatment ranges from 3,375 UAH to 3,710 UAH. This is under the condition that drugs from well-known European manufacturers are not used, which would significantly increase expenses. 4 courses are conducted every 2 weeks, so the minimum total cost ranges from 13,500 UAH to 14,840 UAH.
Doxorubicin and cyclophosphamide are drugs with moderate emetogenicity, requiring the prescription of antiemetic agents for at least the first three days [22]. Thus, 8 mg of ondansetron and 8 mg of dexamethasone are administered before the start of each chemotherapy course. For the next three days, the patient should receive 8 mg of ondansetron intravenously or orally and 4 mg of dexamethasone intramuscularly. According to tabletki.ua website, the minimum cost of dexamethasone is 28 UAH for 5 ampoules of 4 mg each, which is precisely what is needed for 1 course of treatment. According to the same site, ondansetron costs 30 UAH for 5 ampoules of 4 mg and 100 UAH for 10 tablets of 8 mg. As we can see, antiemetic therapy will increase the cost of 1 course by approximately 150 UAH and the cost of 4 courses accordingly by 600 UAH. Roughly an additional 950 UAH per course is needed for filgrastim, as the dose-dense regimen has pronounced hematological toxicity, and colony-stimulating factors are indispensable to ensure the recovery of neutrophil counts before the next course. A more effective drug is pegylated filgrastim; however, at the time of preparing this material, the drug was not available in Ukraine.
Thus, the cost of providing chemotherapy drugs and supportive medications for 4 courses of dose-dense therapy in the AC regimen will range from 15,050 UAH to 15,940 UAH. The following 4 courses of paclitaxel are either 175 mg/m² every 2 weeks or 80 mg/m² weekly for 12 infusions. When administering the drug every 2 weeks, the calculated dose per infusion is 332 mg; with weekly administration, it is 152 mg. Paclitaxel is available in vials of 5 ml (30 mg), 16.67 ml (100 mg), 25 ml (150 mg), 43.33 ml (260 mg), or 50 ml (300 mg). To administer a dose of 332 mg, one should choose either 1 vial of 300 mg or 1 vial of 30 mg (the calculated dose can be rounded without losing efficacy). According to tabletki.ua [18], 1 course will cost 4,416 UAH (300 mg — 3,901 UAH, 30 mg — 515 UAH), and 4 such courses will accordingly cost 17,664 UAH. With weekly infusions at a calculated dose of 152 mg, the minimum cost of paclitaxel for 1 infusion will be 2,481 UAH (1 vial of 100 mg — 1,451 UAH and 2 vials of 30 mg — 1,030 UAH), and for 12 infusions, 29,772 UAH.
Before administering paclitaxel, according to the official instructions [21], premedication with dexamethasone 20 mg intravenously (the minimum price for 20 mg is 28 UAH), diphenhydramine 50 mg (minimum price according to tabletki.ua is 31 UAH for 10 ampoules of 10 mg; for 1 infusion, 5 ampoules are needed, totaling at least 15 UAH), and ranitidine 50 mg (not available in pharmacies at the time of writing) or cimetidine 300 mg (also not available) is mandatory. An alternative to H2-histamine receptor blockers can be proton pump inhibitors, such as 40 mg pantoprazole (the minimum price per vial, according to tabletki.ua [18], is 85 UAH).
Paclitaxel is a low-emetogenic cytostatic [22], so premedication with 8 mg of dexamethasone (from 11 UAH) and 8 mg of ondansetron (12 UAH) is sufficient before each administration, totaling 23 UAH per infusion.
Thus, premedication before each administration of paclitaxel costs 128 UAH, adding 604 UAH to the cost of treatment for 4 courses and 1,812 UAH for 12 weekly infusions. As a result, depending on the chosen dose-dense neoadjuvant chemotherapy regimen with minimal premedication, neoadjuvant treatment costs 18,268 UAH. With the weekly regimen of 12 infusions, the cost increases to 31,584 UAH.
They exclude the provision of syringes, infusion sets (incidentally, an infusion system for paclitaxel adds at least 230 UAH to each course [18]), and solutions for diluting chemotherapeutic agents, chemotherapy drugs and premedication in the dose-dense AC regimen followed by 4 courses of paclitaxel every 2 weeks cost 18,268 UAH. When using AC followed by 12 weekly paclitaxel infusions, the price increases to 46,634 UAH. It should be noted that the cumulative burden on the body with the weekly regimen is less, the therapy is better tolerated, and the complication profile is correspondingly more favorable than with administration every 2 weeks.
Another NCCN-recommended neoadjuvant chemotherapy regimen is TC — docetaxel 75 mg/m² and cyclophosphamide 600 mg/m² intravenously every 3 weeks. The calculated dose of docetaxel per course is 142 mg, which can be provided with 2 vials of 80 mg at a minimum cost of 750 UAH each (1,500 UAH per course) (prices from tabletki.ua). Without such packaging, the cost per course will significantly increase. For instance, 1 vial of 20 mg costs at least 672 UAH, and 4 vials will accordingly cost 2,688 UAH. The cost of cyclophosphamide, as mentioned above, is at least 1,980 UAH per course. Combining docetaxel with cyclophosphamide is moderately emetogenic, adding at least 150 UAH per course for premedication. This combination also frequently leads to clinically significant neutropenia, requiring colony-stimulating factors (at least 950 UAH per course) for prevention or treatment. Thus, the cost of 1 course of treatment under the TC regimen, including minimal supportive therapy, is 4,580 UAH; 4 courses will cost 18,320 UAH, and 6 courses will cost 27,480 UAH.
Calculating additional costs for managing side effects is extremely difficult, as the need for interventions is determined individually. With centralized procurement of medicines by state institutions and hospitals, drug prices may be significantly lower. Today, for neoadjuvant endocrine therapy of hormone-sensitive tumors, either aromatase inhibitors or tamoxifen in monotherapy can be used. Preference is given to the former, as they have demonstrated better results in clinical studies. For hormone therapy in premenopausal patients, aromatase inhibitors must be used alongside ovarian suppression with goserelin or triptorelin [5].
Aromatase inhibitors available on the Ukrainian pharmaceutical market include the non-steroidal letrozole and anastrozole and the steroidal drug exemestane. Randomized clinical trials have shown that none of these drugs is superior to the others [5]; therefore, in actual clinical practice, any non-steroidal drug (letrozole or anastrozole) or the steroidal drug exemestane can be used for neoadjuvant treatment. According to tabletki.ua, the prices are for letrozole 2.5 mg (30 tablets) from 497 UAH, for anastrozole 1 mg (28 pills) from 352 UAH, and for exemestane 25 mg from 700 UAH.
Using synthetic analogs of natural luteinizing hormone-releasing hormone in reproductive-age women for ovarian suppression requires additional expenses. For example, the cost of a 3.6 mg goserelin implant, which provides an effect for 4 weeks, is 2,235 UAH, and the 10.8 mg depot, effective for 12 weeks, is 5,593 UAH. Triptorelin suspension 3.75 mg, providing ovarian ablation for 4 weeks, costs 2,230 UAH, and 11.25 mg, effective for 12 weeks, costs 5,985 UAH.
Vitamin D3 is usually recommended to reduce the toxicity of endocrine drugs (primarily bone-joint drugs). At a dose of 2,000 IU, it can be safely used without laboratory monitoring. According to tabletki.ua, it costs 70 UAH for 30 tablets or 100 UAH for 60 tablets.
Bone resorption inhibitors are also successfully used to correct bone toxicity. The appropriateness and frequency of their use (once every 3–6 months to reduce bone resorption manifestations) are determined individually based on each patient’s bone-joint characteristics. The cost of 4 mg of zoledronic acid, according to tabletki.ua, is 756 UAH. Its administration requires the patient to be in the hospital, at least in a day hospital setting, although the intravenous infusion procedure takes only 15 minutes. An alternative is the oral drug ibandronic acid, which costs 1,508 UAH for 3 tablets. Considering that the drug is taken once per treatment cycle (once every 4 weeks), the cost per tablet is just over 500 UAH, and its use does not require a doctor’s visit.
Thus, for menopausal patients, hormone therapy plus supportive therapy costs, depending on the drug choice, from 997 UAH for letrozole, from 992 UAH for anastrozole, and from 1,270 UAH for exemestane. In premenopausal women, adding goserelin increases the treatment cost by 2,235 UAH per month and triptorelin by 2,230 UAH per month.
Both chemotherapy and endocrine therapy require regular laboratory monitoring, at a minimum, a complete blood count, and liver and kidney function tests. When using dose-dense chemotherapy, laboratory checks are necessary at least one week after cytostatic infusion and before the next course. With endocrine therapy, there is no urgent need for constant laboratory monitoring. Blood tests can be conducted once every 2–3 courses of treatment or more frequently if there are individual indications. Commercial laboratories provide quality laboratory monitoring of clinical (general) and biochemical blood tests starting from a minimum of 1,000 UAH per examination. Prices may vary depending on technology, reagent costs, etc.
As of April 1, 2024, the minimum hourly wage, according to the Ministry of Finance of Ukraine, was 48 UAH per hour [23]. Thus, assuming a 6-hour workday, she loses at least 288 UAH each day that a patient is undergoing treatment. Suppose we consider the average salary published by the Ministry of Finance for June 2024, which is 18,806.63 UAH [24]; then, based on a 36-hour workweek [25], each working hour in that same June cost approximately 130 UAH (from an average calculation of 145 working hours per month with a 36-hour workweek). Therefore, for each working day missed due to hospitalization, the patient loses about 780 UAH. Even with compensation for losses from the Social Insurance Fund, the overall losses from inpatient treatment are significant.
Moreover, a patient receiving chemotherapy usually cannot return to work immediately after discharge from the hospital, so she continues outpatient treatment, remaining on sick leave for at least several more days. The number of such days depends on the patient’s condition, the severity of chemotherapy side effects, and each specific patient’s activity type. According to the most modest estimates, being on sick leave for one week resulted in an average loss of about 5,500 UAH.
Unlike chemotherapy, endocrine therapy does not require hospitalization; in the absence of pronounced side effects, visiting the doctor once every 2–3 months is sufficient. Therefore, the cost of one working day every 2–3 months, on average 780 UAH, almost does not affect the patient’s losses. Moreover, the patient can often arrange to make up work hours on other days or times, thus not incurring any financial losses due to reduced wages.
To date, the optimal duration of neoadjuvant endocrine therapy remains undetermined. To ensure the possibility of performing the organ-preserving treatment, it should be at least 4 months, but extending the treatment generally contributes to improved outcomes [5].
Considering the above analysis, we can calculate the minimum direct and indirect treatment costs. The direct treatment costs include the base rate for readiness to provide medical care, the total cost of antitumor therapy, supportive therapy, and laboratory tests.
The base rate for the readiness to provide inpatient medical care to one person over a year, taking into account the adjustment coefficient, is 35,703 UAH per year, and for outpatient care, 25,765 UAH per year. For further calculations, these figures will be rounded to whole numbers.
The total cost of neoadjuvant chemotherapy in the dose-dense regimen of 4 courses of AC followed by 4 courses of paclitaxel every 2 weeks, taking into account the necessary premedication and provided there are no treatment complications, and excluding the cost of solutions for diluting chemotherapeutic agents, syringes, infusion sets, and other minor expenses, is at least 33,118 UAH. When using 12 weekly paclitaxel infusions, the treatment cost increases to 46,634 UAH. The cost of 4 courses of chemotherapy according to the TC regimen is 18,320 UAH, and for 6 courses, 27,480 UAH.
The minimum cost of 4 courses of endocrine neoadjuvant therapy (1 course = 4 weeks), including supportive therapy, in postmenopausal women is 3,988 UAH for letrozole, 3,968 UAH for anastrozole, and 5,080 UAH for exemestane. The use of goserelin in premenopausal women will increase the treatment cost to 12,928 UAH for letrozole, 12,908 UAH for anastrozole, and 14,020 UAH for exemestane.
Another cost indicator, which can be either planned or situational depending on the current necessity and, in our opinion, can be considered indirect, is laboratory testing, with prices starting from 1000 UAH per test. For patients receiving chemotherapy, such tests are conducted at least twice per treatment course and over 8 courses; this amounts to 16 or more times. The total cost for laboratory tests thus exceeds 16,000 UAH. For patients receiving endocrine therapy, it’s only 3–4 tests or fewer. The amount needed for laboratory tests rarely exceeds 4,000 UAH for 4–6 four-week courses of treatment. Indirect costs include a loss of about 5,500 UAH each week on sick leave.
Costs associated with decreased quality of life, emotional and physical experiences related to anticipating treatment, and negative phenomena during treatment, including the need for additional minimally invasive interventions, examinations, hair loss, changes in appetite, social behavior, etc., cannot be calculated. Special tests, questionnaires, and the like are used for this.
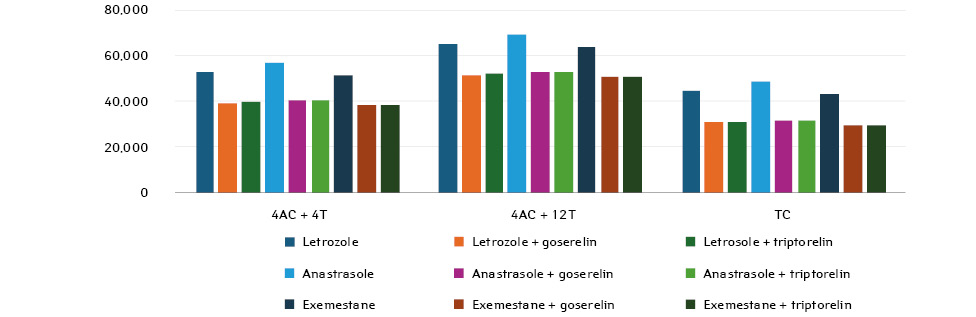
Considering the conducted analysis, the cost-minimization analysis (CMA) indicator was calculated for patients receiving neoadjuvant chemotherapy compared to those receiving endocrine therapy (Tables 1–2, Figure). For convenience of calculation, considering that chemotherapy can last up to 6 courses, the costs for hormone therapy were also calculated for 6 classes.
| Neoadjuvant chemotherapy (DC1) | Neoadjuvant hormone therapy (DC2) | |||||
|---|---|---|---|---|---|---|
| 4АС+4Т | 4АС+
12Т |
TC | Letrozole | Anastrozole | Exemestane | |
| Base Rate (UAH) | 35,703 | 35,703 | 35,703 | 25,765 | 25,765 | 25,765 |
| Minimum cost of anticancer drugs | 28,164 | 43,272 | 27,480 | 2,9821
16,3922 16,3633 |
2,1121
15,5222 15,4923 |
4,2001
17,6102 17,5803 |
| Minimum cost of premedication / support | 5,004 | 6,212 | 1,100 | 3,436 | 3,436 | 3,436 |
| Total DS | 68,871 | 85,187 | 64,283 | 32,1831
45,5932 45,5643 |
27,8771
44,7232 44,6933 |
33,3711
46,8112 46,7813 |
Notes. An explanation of costs is provided in the text:
1Endocrine monotherapy in postmenopausal patients.
2Endocrine therapy with ovarian suppression using goserelin in premenopausal patients.
3Endocrine therapy with ovarian suppression using triptorelin in premenopausal patients.
| Neoadjuvant chemotherapy (ІС1) | Neoadjuvant hormone therapy (ІС2) | |||||
|---|---|---|---|---|---|---|
| 4АС+4Т | 4АС+12Т | 6ТС | Letrozole | Anastrozole | Exemestane | |
| Laboratory monitoring | 16,000 | 16,000 | 12,000 | 3,0001 | 3,0001 | 3,0001 |
| Incapacity | 5,500 | 5,500 | 5,500 | 2,340 | 2,340 | 2,340 |
| Total AC | 21,500 | 21,500 | 12,500 | 5,340 | 5,340 | 5,340 |
Notes. Explanations of costs are provided in the text:
1Calculation for one laboratory test every 2 courses.
2Average cost of 3 working days over 6 treatment cycles when the patient is absent from work due to doctor visits.
The maximum direct treatment costs are required when using the dose-dense regimen of 4 courses of AC every 2 weeks plus 12 weekly infusions of paclitaxel, and based on calculations of minimum prices, amounted to 85,187 UAH. The minimum direct cost needed for 6 courses of neoadjuvant hormone therapy with anastrozole in postmenopausal patients is 27,877 UAH. In premenopausal and perimenopausal women, the use of synthetic analogs of GnRH significantly increases direct treatment costs. Thus, 6 courses of neoadjuvant hormone therapy, taking into account all components of direct costs, with anastrozole and goserelin require a minimum of 44,723 UAH, and with triptorelin, 44,693 UAH (Table 1).
Indirect costs for dose-dense regimens combining doxorubicin with cyclophosphamide followed by paclitaxel courses, both every 2 weeks and weekly, amount to about 21,500 UAH, and chemotherapy with docetaxel and cyclophosphamide is approximately 17,500 UAH (Table 2).
Overall, as calculations show, the costs for a dose-dense combination of doxorubicin 60 mg/m² in combination with cyclophosphamide 600 mg/m² every 2 weeks for 4 courses, followed by paclitaxel 175 mg/m² every 2 weeks for 4 classes, amount to from 90,371 UAH. Another modification of the dose-dense regimen, where AC is conducted as in the previous variant and paclitaxel is administered at 80 mg/m² weekly for 12 infusions, requires 102,684 UAH. 6 courses of the TC regimen (docetaxel 75 mg/m² in combination with cyclophosphamide 600 mg) involve costs starting from 81,783 UAH.
The cost of hormone therapy is significantly lower; however, it closely depends on the patient’s reproductive status. Postmenopausal women receive one of the aromatase inhibitors without adding ovarian suppressors. 6 courses of letrozole 2.5 mg daily are required from 37,523 UAH, anastrozole from 33,217 UAH, and exemestane from 38,711 UAH. Women in pre- and perimenopause need the use of synthetic GnRH analogs, which increases the cost of treatment. For instance, when using a 4-week goserelin depot, the cost of 6 courses of letrozole increases to 50,933 UAH, anastrozole to 50,063 UAH, and exemestane to 52,151 UAH. Adding a 4-week triptorelin depot increases the price of 6 courses of treatment with letrozole to 50,904 UAH, anastrozole to 50,033 UAH, and exemestane to 52,121 UAH. The cost of dose-dense treatment with 4 courses of chemotherapy with doxorubicin and cyclophosphamide followed by 4 courses of dose-dense paclitaxel is higher by 52,848 UAH compared to letrozole monotherapy, by 57,154 UAH compared to anastrozole, and by 51,660 UAH compared to exemestane. The costs of 4 courses of dose-dense treatment with doxorubicin and cyclophosphamide followed by 12 weekly infusions of paclitaxel will be significantly higher, amounting to 65,161 UAH more compared to letrozole, 69,467 UAH more compared to anastrozole, and 63,973 UAH more compared to exemestane.
Somewhat lower, but still significant, are the costs when adding synthetic GnRH analogs to aromatase inhibitors. For example, the difference in the price of treatment with 4 courses of chemotherapy with doxorubicin and cyclophosphamide followed by 4 courses of dose-dense paclitaxel, when adding goserelin, will be from 39,434 UAH, and when adding triptorelin, 39,467 UAH. Treatment with anastrozole and goserelin will be cheaper by 40,308 UAH and with triptorelin by 40,338 UAH. Adding these same drugs to exemestane will be more affordable by 38,220 and 38,250 UAH, respectively.
Treatment with 4 courses of dose-dense doxorubicin and cyclophosphamide followed by 12 weekly infusions of paclitaxel will be more expensive by 51,749 UAH than treatment with anastrozole and goserelin and by 51,780 UAH when adding triptorelin to anastrozole. Similarly, combinations of anastrozole with goserelin and triptorelin will cost less by 52,621 and 52,651 UAH, respectively, and combinations of exemestane with these exact GnRH analogs by 50,553 and 50,563 UAH, respectively. Again, the cost difference favors hormone therapy when comparing the treatment cost of exemestane with the corresponding GnRH analogs to treatment with docetaxel and cyclophosphamide: for anastrozole with goserelin, 30,850 UAH; with triptorelin, 30,879 UAH; for anastrozole, 31,720 UAH with goserelin and 31,750 UAH with triptorelin; and exemestane with goserelin will be cheaper by 28,632 UAH, with triptorelin by 29,662 UAH (Figure).
Conclusions
Neoadjuvant endocrine therapy for hormone-dependent (including luminal B HER2/neu-negative) BC can be considered an adequate alternative to neoadjuvant chemotherapy. It not only provides a similar opportunity to perform organ-preserving surgical interventions but also allows for significant cost savings in treatment, which is extremely important in the difficult economic conditions caused by the war in Ukraine. Depending on the choice of drugs for endocrine therapy, compared to internationally recommended neoadjuvant chemotherapy regimens, the savings range from about 30,000 UAH to about 70,000 UAH. However, one should not rely solely on the results of pharmacoeconomic calculations, as long-term treatment outcomes have not yet been thoroughly studied. Therefore, when choosing a neoadjuvant treatment strategy, a multidisciplinary team should consider a multifactorial analysis of each patient.
Information on conflict of interest: the authors declare no conflict of interest.
REFERENCES
1. World Cancer Research Fund International. Breast cancer statistics. Retrieved from http://www.wcrf.org/cancer-trends/breast-cancer-statistics/?form=MG0AV3.
2. Федоренко, З. П., Сумкіна, О. В., Горох, Є. Л., & Гулак, Л. О. (2024). Рак в Україні, 2022–2023. Захворюваність, смертність, показники діяльності онкологічної служби. Бюлетень Національного канцер-реєстру України. (Vol. 25). Кропивницький: Поліум.
3. Федоренко, З. П., Сумкіна, О. В., Горох, Є. Л., & Гулак, Л. О. (2023). Рак в Україні, 2021–2022. Захворюваність, смертність, показники діяльності онкологічної служби. Бюлетень Національного канцер-реєстру України. (Vol. 24). Кропивницький: Поліум.
4. DePolo, J. Molecular Subtypes of Breast Cancer. Types of Breast Cancer. Retrieved from http://www.breastcancer.org/types/molecular-subtypes.
5. Завізіон, В. Ф., & Артеменко, М. В. (2024). Неоад’ювантна ендокринна терапія раку молочної залози: історія та сучасні погляди на проблему (огляд літератури). Клінічна онкологія, 14, 3(55), 275–283. doi: 10.32471/clinicaloncology.2663-466X.55-3.32929.
6. NCCN Clinical Practice Guidelines in Oncology. (2024). Breast Cancer. NCCN Guidelines®. Version 5.2024. Retrieved from http://www.nccn.org/professionals/physician_gls/pdf/breast.pdf.
7. Park, K. H., Loibl, S., Sohn, J., Park, Y. H., Jiang, Z., Tadjoedin, H., … Harbeck, N. (2024). Pan-Asian adapted ESMO Clinical Practice Guidelines for the diagnosis, treatment, and follow-up of patients with early breast cancer. ESMO Open, 9(5), 102974. doi: 10.1016/j.esmoop.2024.102974.
8. Korde, L. A., Somerfield, M. R., Carey, L. A., Crews, J. R., Denduluri, N., Hwang, E. S., & Hershman, D. L. (2021). Neoadjuvant Chemotherapy, Endocrine Therapy, and Targeted Therapy for Breast Cancer: ASCO Guideline. Journal of Clinical Oncology, 39(13), 1485–1505. doi: 10.1200/JCO.20.03399.
9. Andre, F., Ismaila, N., Allison, K. H., Barlow, W. E., Collyar, D. E., Damodaran, S., … Stearns, V. (2022). Biomarkers for Adjuvant Endocrine and Chemotherapy in Early-Stage Breast Cancer: ASCO Guideline Update. Journal of Clinical Oncology, 40(16), 1816-1837. doi: 10.1200/JCO.22.00069.
10. Exemestane, Letrozole, or Anastrozole in Treating Postmenopausal Women Who Are Undergoing Surgery for Stage II or Stage III Breast Cancer. Retrieved from ctv.veeva.com/study/ exemestane-letrozole-or-anastrozole-in-treating-postmenopausal-women-who-are-undergoing-surgery-fo.
11. Sirico, M., Virga, A., Conte, B., Urbini, M., Ulivi, P., Gianni, C., … Schettini, F. (2023). Neoadjuvant endocrine therapy for luminal breast tumors: State of the art, challenges and future perspectives. Critical Reviews in Oncology. Hematology, 181, 1040–8428. doi: 10.1016/j.critrevonc.2022.103900.
12. Tran, B., & Bedard, P. L. (2011). Luminal-B breast cancer and novel therapeutic targets. Breast Cancer Research, 13, 221. doi: 10.1186/bcr2904.
13. Zanuso, V., Fregoni, V., & Gervaso, L. (2020). Side Effects of Adjuvant Chemotherapy and their Impact on Outcome in Elderly Breast Cancer Patients: A Cohort Study. Future Science OA, 6(9), FSO617. doi: 10.2144/fsoa-2020-0076.
14. Aldaak, M., Suliman, H. M., Abd-Elgadir, E. E., & Abdoon, I. H. (2022). Impact of anticancer therapy on the quality of life of Sudanese patients with breast cancer at Khartoum oncology hospital. BMC Women’s Health, 22(1), 448. doi: 10.1186/s12905-022-02041-0.
15. Яковлєва, Л. В., & Міщенко О. Я. Фармакоекономічний аналіз. Фармацевтична енциклопедія. Відновлено з http://www.pharmencyclopedia. com.ua/ article/288/farmakoekonomichnij-analiz.
16. Яковлєва, Л. В., & Ткачова, О. В. Витрати у фармакоекономіці. Фармацевтична енциклопедія. Відновлено з http://www.pharmencyclopedia. com.ua/article/1735/vitrati-u-farmakoekonomici.
17. Посібник програми медичних гарантій 2024: відновлення і розвиток. (2024). Національна служба здоров’я України. Відновлено з vaccine.org.ua/wp-content/uploads/2024/06/posibnyk_pmg_2024.pdf.
18. Сервіс пошуку та бронювання ліків в Україні. Відновлено з tabletki.ua.
19. Пошук ліків в аптеках, ціни на ліки в аптеках України. Відновлено з medbrowse.com.ua.
20. Аптека 911. (n.d.). Перелік ліків за категоріями. Відновлено з apteka911.ua/ ua.
21. ГО «Ліки Контроль». (n.d.). Ліки Контроль. Відновлено з likicontrol.com.ua.
22. Локальний протокол медичної допомоги та клінічний маршрут хворих з еметичним синдромом. Відновлено з unci.org.ua/standarty-diagnostyky-ta-likuvannya.
23. Мінімальна зарплата в Україні. (2024). Мінімальна зарплата в Україні з 2000 по 2024 рр. Відновлено з index.minfin.com.ua/ua/labour/salary/min.
24. Середня заробітна плата за даними ПФУ. (2024). Середня місячна зарплата за даними ПФУ в 2024 р. Відновлено з index.minfin. com.ua/ua/labour/salary/average/pfu/2024/.
25. Норми тривалості робочого часу на 2021 рік (2021). Бухгалтер 911. Відновлено з buhgalter911.com/spravochniki/oplata-truda/ norma-prodolzhitelnosti-rabochego-vremeni/ norma-prodolghitelynosti-rabochego-950661.html.
Correspondence:
Viktor Zavizion
31 Blyzhnia str., Dnipro, 49102
Dnipro State Medical University
E-mail: kafedraradonco@gmail.com
Адреса для листування:
Завізіон Віктор Федорович
49102, Дніпро, вул. Ближня, 31
Дніпровський державний медичний університет
E-mail: kafedraradonco@gmail.com














Leave a comment