A case of superficially spreading melanoma associated with an intradermal nevus
Voloshynovych M.1, Boichuk T.2, Matkovska N.1, Tkach V.1, Voloshynovych V.1, Kozak N.1
Summary. The way melanomas appear has been of considerable interest to researchers for many years. At the current stage of research, the data indicating that this tumour arises de novo, rather than as a result of transformation of a pre-existing skin lesion, are overwhelming. Therefore, cases of melanoma-associated nevi are of considerable clinical and diagnostic interest. The vast majority of such tumours are associated with various types of pigmented nevi, while there are only isolated sporadic descriptions of the transformation of intradermal nevi into melanoma. The publication presents a clinical case of this rare pathology. There are data from clinical examination and dermoscopic examination. The lesion was excised within healthy tissue. Pathohistological study of the material was carried out. The diagnosis of superficially spreading melanoma against the background of intradermal nevus was confirmed. Melanocytes from the epidermis spread into the papillary and reticular layers of the dermis to a maximum depth of 1.4 mm. To clarify the depth of invasion, immunohistochemistry was performed, Breslow 1.0 mm. To exclude microsatellite metastases, re-excision of the site of the previous intervention was performed. The pathohistological structure of the material was typical for a postoperative scar, no signs of tumour growth were detected. The complex visual and dermoscopic structure of associated melanomas can lead to misdiagnosis. The deep location of the primary lesion requires the use of immunohistochemistry to determine the thickness of the tumour. High-quality diagnosis directly affects the further management of the patient.
Received 14.02.2024
Accepted for publication 16.02.2024
DOI: 10.32471/clinicaloncology.2663-466X.53-1.31796
Introduction
The way melanomas appear has been of considerable interest to researchers for many years. At the current stage of research, the data indicating that this tumour arises de novo, rather than as a result of transformation of a pre-existing skin lesion, are overwhelming. Therefore, cases of nevus-associated melanomas (NAMs), the incidence of which, according to the results of many multicentre studies, ranges from 20 to 30%, are of considerable clinical and diagnostic interest [1–3].
A statistical analysis of the information indicates that NAMs occur more often in young people, in the trunk area, and are usually represented by a smaller tumour thickness according to Breslow [4].
However, the vast majority of NAMs are associated with various types of pigmented nevi, while there are only a few sporadic reports of the transformation of intradermal nevi into melanoma [5–7].
Case Synopsis
Patient A, 43 years old, consulted a dermatologist with complaints of papillomas on the hands. She had Fitzpatrick skin phototype 2, a history of melanoma in blood relatives, and a history of repeated sunburns. A routine examination of the skin surface revealed a solitary papular rash on the left shoulder blade with a heterogeneous colour (Fig. 1a).
Digital dermoscopy with photofixation (FotoFinder Medicam 1000s camera in polarisation mode) was performed. Due to the complex appearance of the lesion, an ultrasound gel was additionally applied to the skin surface. The lesion is heterogeneous, with convex (Fig. 1b) and flat parts (Fig. 1c).

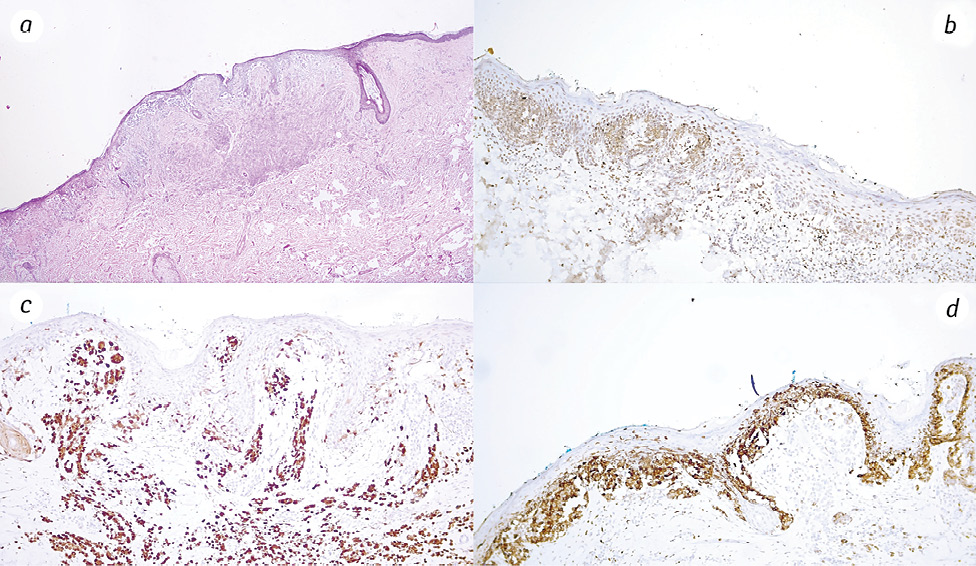
The tumour was excised within healthy tissue. A pathohistological study of the material was carried out. The diagnosis of superficially spreading melanoma against the background of an intradermal nevus was confirmed. Melanocytes from the epidermis spread into the papillary and reticular layers of the dermis, to a maximum depth of 1.4 mm (Fig. 2a). To clarify the depth of invasion, immunohistochemistry was performed (PRAME, p16, HMB-45) — Clarks Level 4, Breslow stage II (1.0 mm) (Fig. 2b–2d).
To exclude microsatellite metastases, the site of the previous intervention was re-excised. The pathohistological structure of the material was typical for a postoperative scar, and no signs of tumour growth were detected. The patient is under the supervision of a family doctor and undergoes periodic follow-up examinations by a dermatologist.
Case Discussion
In the case of NAMs arising from an intradermal nevus, the thickness of tumours may be incorrectly determined due to the deep location of the primary lesion, and the presence of a convex part of the tumour leads to a false diagnosis of nodular melanoma.
The complex dermoscopic structure requires detailed consideration. The papular part, where vascular elements are observed in the centre of the skin-coloured parts, is suggestive of an intradermal nevus, but such vessels visible on an erythematous background can also be observed in melanoma (Fig. 1b) [8]. The central area contains multiple white lines and single vascular inclusions, which may have arisen as a result of scarring or tumour regression. On the periphery, the pigment grid of a typical nevus structure is interspersed with areas of grey-blue and brown structureless zones, pigment inclusions, branched lines, and negative pigment grid, which are signs of dysplasia (Fig. 1c). In this case, in addition to the heterogeneous structure, the signs of NAMs may include areas of negative pigmentation and, structureless brown zones, which are more common in transforming lesions rather than de novo [9].
Conclusion
NAMs are usually associated with different types of pigmented nevi, whereas the transformation of intradermal nevi into melanoma is a rare case. Complex visual and dermoscopic structure can lead to a false diagnosis. Deep location of the primary lesion requires the use of immunohistochemistry to determine the thickness of the tumour. High-quality diagnostics directly affects the further tactics of patient management.
References
1. Wiggins, J., & Polsky, D. (2021). Melanoma origins: data from early‐stage tumours supports de novo and naevus‐associated melanomas as distinct subtypes. The British Journal of Dermatology, 185(1), 9–10. doi.org/10.1111/bjd.20396.
2. Dessinioti, C., Befon, A., & Stratigos, A. J. (2023). The association of nevus-associated melanoma with common or dysplastic melanocytic nevus: A systematic review and meta-analysis. Cancers, 15(3), 856. doi.org/10.3390/cancers15030856.
3. Dessinioti, C., Geller, A. C., & Stratigos, A. J. (2022). A review of nevus‐associated melanoma: What is the evidence? Journal of the European Academy of Dermatology and Venereology: JEADV, 36(11), 1927–1936. doi.org/10.1111/jdv.18453.
4. Dessinioti, C., Geller, A. C., Stergiopoulou, A., Dimou, N., Lo, S., Keim, U., … Stratigos, A. J. (2021). A multicentre study of naevus‐associated melanoma vs. de novo melanoma, tumour thickness and body site differences. British Journal of Dermatology, 185(1), 101–109. doi.org/10.1111/bjd.19819.
5. Drvar, L., Radoš, D., Manola, J., Mataić, I., Dotlić, A., & Krušlin, S. (2023). Melanoma Developing from an Intradermal Nevus: Report on Two Patients. Acta Dermatovenerol Croat, 31(1), 40–42.
6. Arjona-Aguilera, C., Gil-Jassogne, C., Jiménez-Gallo, D., & Albarrán-Planelles, C. (2015). Melanoma intradérmico asociado a nevo melanocítico intradérmico. Actas Dermo-sifiliograficas, 106(9), 776–777. doi.org/10.1016/j.ad.2015.04.016.
7. Nakai, N., & Katoh, N. (2015). Melanoma arising from the epidermis overlying an acquired intradermal nevus on the forehead. Indian Journal of Dermatology, Venereology and Leprology, 81(5), 533. doi.org/10.4103/0378-6323.158653.
8. Rosendahl, C. (2023). Marozava Dermatoscopy and Skin Cancer: A handbook for hunters of skin cancer and melanoma. Scion Publishing, Updated edition, 686.
9. Reiter, O., Kurtansky, N., Nanda, J. K., Busam, K. J., Scope, A., Musthaq, S., & Marghoob, A. A. (2021). The differences in clinical and dermoscopic features between in situ and invasive nevus‐associated melanomas and de novo melanomas. Journal of the European Academy of Dermatology and Venereology: JEADV, 35(5), 1111–1118. doi.org/10.1111/jdv.17133.
Correspondence:
Marian Voloshynovych
16, Kropyvnyckoho, Ivano-Frankivsk, 76000, Ukraine
Ivano-Frankivsk National Medical University
E-mail: mvoloshynovych@gmail.com
Адреса для листування:
Мар’ян Волошинович
76000, м. Івано-Франківськ, вул. Кропивницького, 16, Україна
Івано-Франківський національний медичний університет
E-mail: mvoloshynovych@gmail.com














Leave a comment